Dean Katherine Gregory meets with Jason Luu ’24 and Sabrina Ng ’23 in CSON’s student lounge. Photograph: Lee Pellegrini.
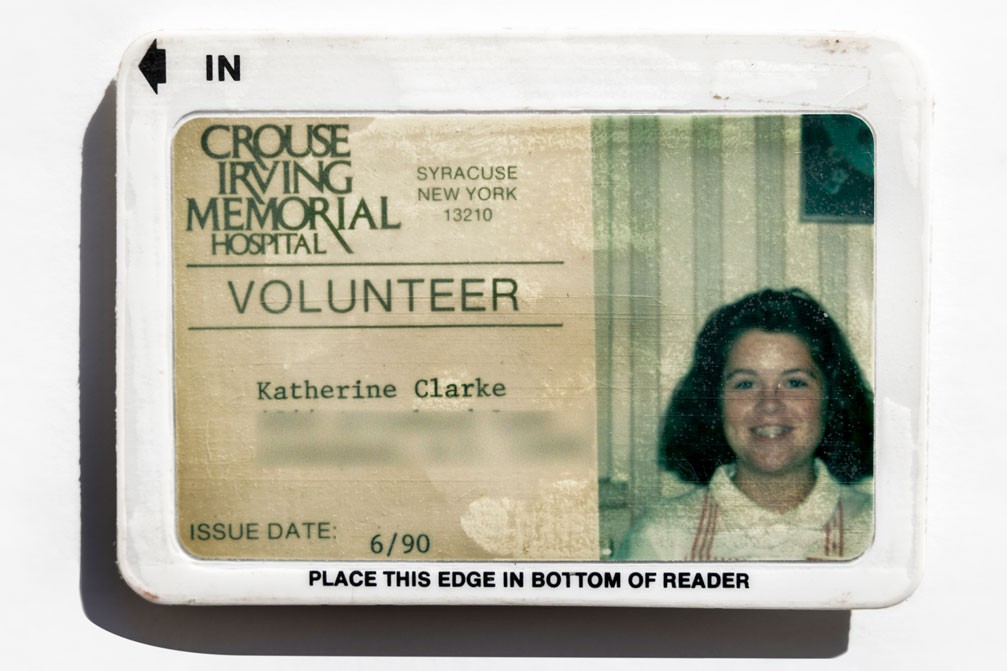
Shortly after being named dean of the Connell School of Nursing (CSON), Katherine E. Gregory was intrigued to learn that she is the eighth person to assume the role since the school’s founding in 1947. “Eight is considered a fortuitous number in many cultures of the world,” says Gregory. “It’s a sign of good luck and a sign of balance. Coming out of the pandemic, I think we really need both for our school, and in the profession of nursing.”
While she can only hope for good luck, Gregory has a vision for the future of nursing and a diversity of experience as a clinician, scientist, and leader that make her uniquely qualified to promote a sense of balance and equanimity as she guides CSON through the time of change that lies ahead.
She succeeds Susan Gennaro, who stepped down as dean last spring after 13 years. But Gregory’s arrival to Chestnut Hill is really a return: she received a doctorate in nursing at CSON in 2005 and taught on the school’s faculty from 2006–2014.
“I’m really excited to be back in this wonderful and vibrant place,” says Gregory, seated in her Maloney Hall office at a table decorated with orchids in a vase, a welcome gift from the school. “The faculty and staff are highly engaged and we have the best students anyone could ask for.”