By
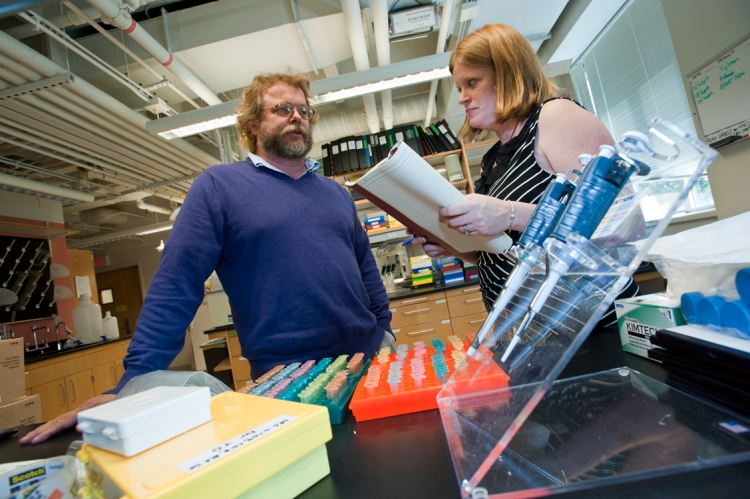
A small molecule continues to speak volumes about the devastating impact of HIV infection on the health of patients living longer lives through the successful use of antiretroviral drugs, according to new research from the lab of Professor of Biology Ken Williams.
In a recent study, the molecule – known as CD163 – helped Williams and colleagues from Harvard Medical School make the connection between body’s immune system response and the increased incidence of cardiovascular disease among people living with HIV, according to a report in the Journal of the American Medical Association.
Known as a scavenger receptor, CD163 is shed during the activation of monocyte and macrophage cells as part of the body’s immune response to HIV infection. Dispatched by the immune system to combat infection, monocytes enter tissue and exit as macrophage cells. In earlier research, Williams and his lab have shown CD163, a protein molecule within these infection-fighting cells, serves as a valuable biomarker for the effectiveness of HIV antiretroviral (ARV) therapies.
The new study of 80 HIV-positive patients demonstrated for the first time that arterial inflammation occurs at a 60 percent higher rate in HIV-infected patients compared to non-HIV patients with similar risk profiles.
Three-dimensional images obtained through PET imaging revealed telltale CD163 and macrophage infiltration in arterial walls susceptible to rupture. In addition, that arterial wall inflammation in HIV patients increased independent of traditional risk factors, giving further weight to the infiltrative role of activated monocytes and macrophages in the upper aorta.
The findings reveal there is a general activation of the immune system in patients and, in particular, macrophage inflammation in HIV patients that correlates and likely drives cardiac disease, said Williams. This activation persists despite the fact that anti-retroviral therapies successfully halt the progress of HIV.
“What we’re finding in the HIV field is that effective anti-retroviral therapies keep the virus counts low, which is crucial for these patients,” said Williams, whose research is supported by funding from the National Institutes of Health’s National Institute of Neurologic Disorders and Stroke. “But we’re seeing an increased level of chronic immune activation which we can now connect to damaging inflammation and arterial plaque. These are silent killers and it’s crucial we learn as much as we can in order to arrive at new therapies.”
Specifically, patients with HIV display a high prevalence of non-calcified coronary atherosclerotic lesions that are increased in association with markers of macrophage activation. The finding is significant because earlier studies have shown that monocyte and macrophage infiltration of the linings of tiny blood vessels contributes to the development of atherosclerotic plaque that is susceptible to rupture.
The connection between macrophage and monocyte activity and cardiovascular disease sheds new light on the specific links between CVD, the immune system, HIV and antiretroviral therapies, according to the researchers.
While ART drugs have successfully stabilized patients by suppressing many of the deadly effects of HIV and the subsequent onset of AIDS, the Williams lab has shown monocyte and macrophage activity are connected to debilitating illnesses, such as dementia and, now, cardiovascular disease.
In addition to Williams, the research team included BC Research Assistant Professor of Biology Tricia Burdo and Harvard Medical School researchers Sharath Subramanian, Ahmed Tawakol, Suhny Abbara, Jeffrey Wei, Jayanthi Vijayakumar, Erin Corsini, Markella V. Zanni, Udo Hoffmann, Janet Lo and Steven K. Grinspoon.